Mental health billing services play a vital role in ensuring the financial stability of mental health and behavioral health practices. As the demand for mental health care continues to rise, providers face increasing administrative challenges related to billing, coding, compliance, and reimbursements. Unlike general medical billing, mental health billing involves complex payer rules, specialized coding, strict documentation requirements, and frequent regulatory updates.
Professional Mental Health Billing Services help psychiatrists, psychologists, therapists, counselors, and behavioral health clinics streamline their revenue cycle while maintaining compliance and improving cash flow.
Understanding Mental Health Billing
Mental health billing refers to the process of submitting and following up on insurance claims for services provided by mental and behavioral health professionals. These services may include psychiatric evaluations, psychotherapy sessions, counseling, medication management, substance abuse treatment, and tele-mental health services.
Mental health billing differs significantly from standard medical billing due to:
-
Unique CPT and HCPCS codes
-
Time-based therapy coding
-
Mental health parity regulations
-
Telehealth billing requirements
-
Authorization and visit limitations
-
Documentation and compliance standards
Errors in any of these areas can result in claim denials, delayed payments, audits, or legal penalties.
Challenges Faced by Mental Health Providers in Billing
Mental health providers often face multiple billing-related challenges that directly impact revenue:
1. Complex Coding Requirements
Mental health billing uses specific CPT codes such as psychotherapy codes (90832, 90834, 90837), psychiatric diagnostic evaluation codes, and medication management codes. Selecting incorrect codes or mismatched time units can lead to claim rejections.
2. Frequent Claim Denials
Denials may occur due to missing authorizations, eligibility issues, incorrect modifiers, or documentation errors. Behavioral health claims are closely scrutinized by payers.
3. Telehealth Billing Complexity
With the growth of tele-mental health services, billing rules vary by payer and state. Incorrect place-of-service codes or modifiers can result in non-payment.
4. Mental Health Parity Compliance
Mental Health Parity and Addiction Equity Act (MHPAEA) requires insurers to treat mental health services equally to medical services. Non-compliance can result in penalties and payment delays.
5. Administrative Burden
Managing billing in-house consumes time that providers could otherwise dedicate to patient care.
What Are Mental Health Billing Services?
Mental Health Billing Services involve outsourcing billing operations to specialized medical billing experts who understand the complexities of behavioral health revenue cycle management. These services manage the entire billing lifecycle, from patient intake to final reimbursement.
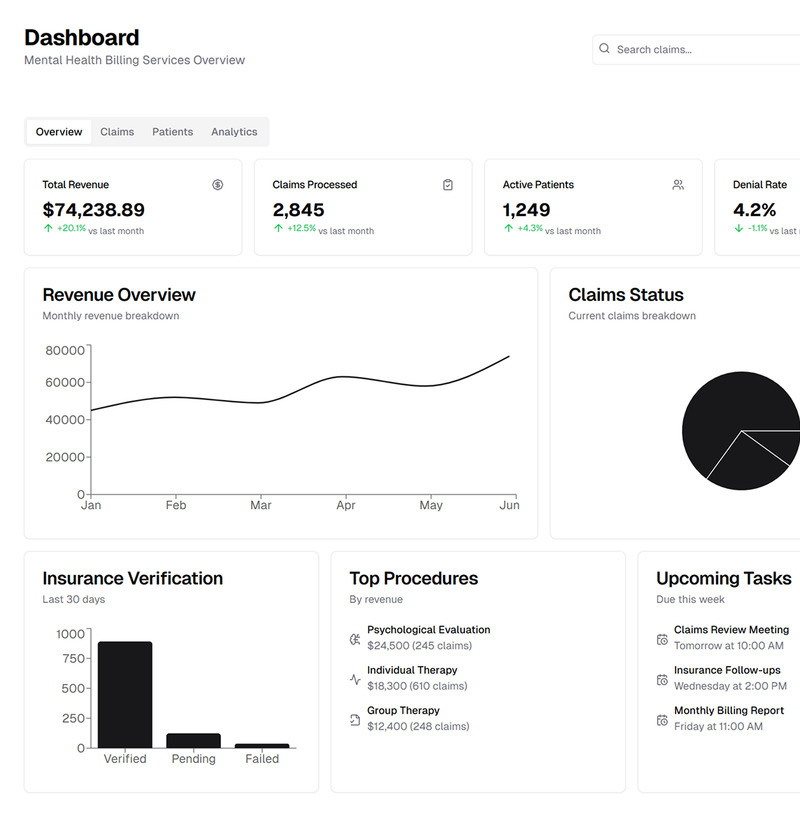
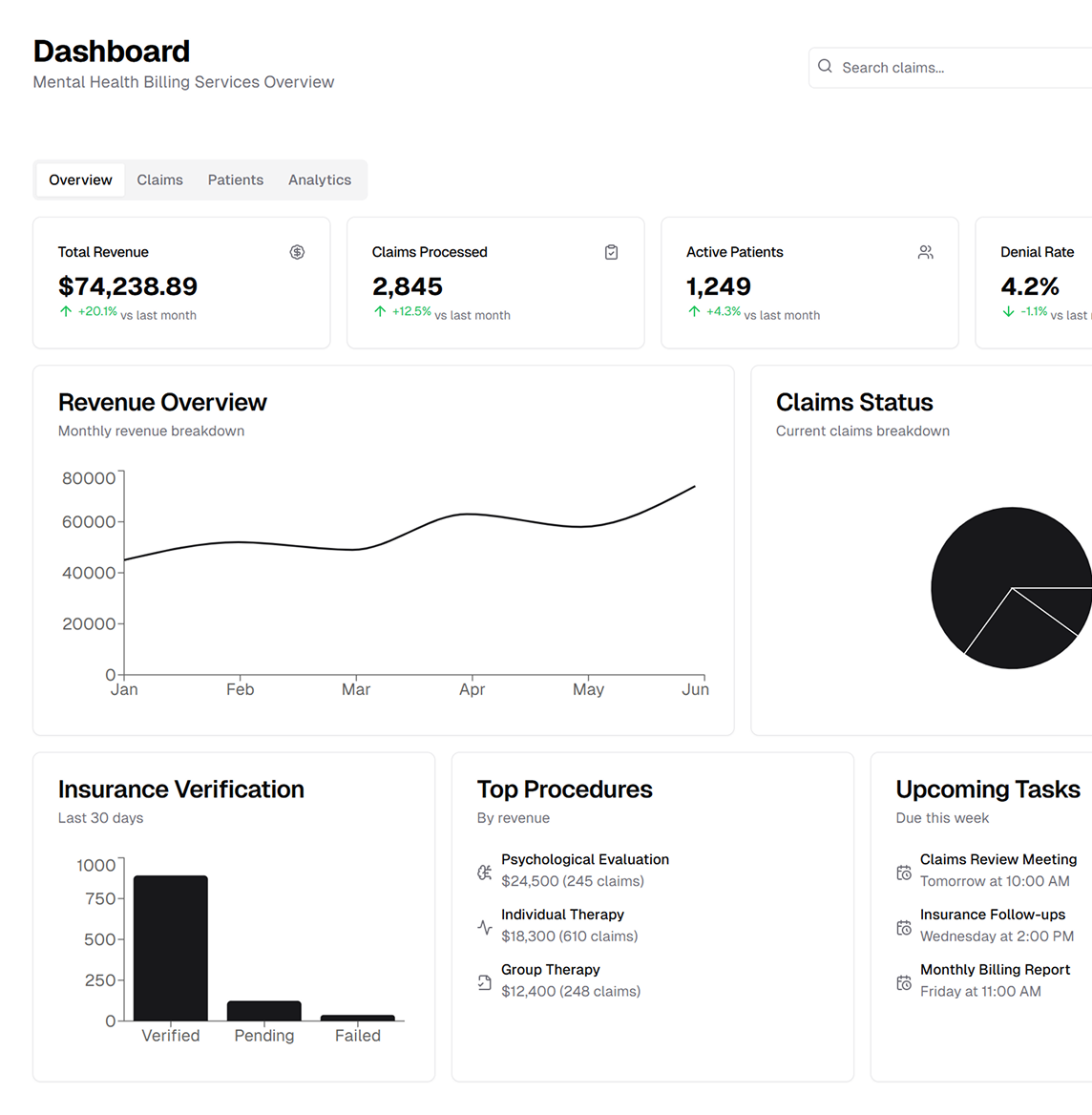
Key Components of Mental Health Billing Services
1. Patient Eligibility and Benefits Verification
Before services are rendered, billing teams verify insurance coverage, mental health benefits, copayments, deductibles, and authorization requirements. This step reduces claim denials and improves patient transparency.
2. Accurate Medical Coding
Certified coders ensure correct CPT, ICD-10, and HCPCS coding based on the provider’s documentation. Proper time-based coding and modifier usage are critical for mental health services.
3. Claim Submission and Tracking
Claims are submitted electronically to insurance payers and monitored throughout the adjudication process. Any rejections are corrected and resubmitted promptly.
4. Denial Management and Appeals
Denied claims are analyzed to identify root causes. Billing specialists prepare and submit appeals with supporting documentation to recover lost revenue.
5. Payment Posting and Reconciliation
Payments from insurance companies and patients are accurately posted. Explanation of Benefits (EOBs) are reconciled to ensure correct reimbursement.
6. Patient Billing and Statements
Clear and compliant patient statements are generated, and patient inquiries are handled professionally to improve satisfaction.
7. Accounts Receivable (AR) Follow-Up
Outstanding claims are followed up regularly to reduce aging AR and improve cash flow.
8. Compliance and Reporting
Mental health billing services ensure compliance with HIPAA, payer guidelines, and federal regulations while providing detailed financial reports.
Benefits of Outsourcing Mental Health Billing Services
Improved Cash Flow
Professional billing services reduce claim denials and accelerate reimbursements, resulting in consistent revenue.
Reduced Administrative Burden
Providers can focus on patient care instead of billing and paperwork.
Higher First-Pass Claim Acceptance Rate
Expert coding and claim submission increase the likelihood of claims being accepted the first time.
Cost Efficiency
Outsourcing eliminates the need for in-house billing staff, training, and software expenses.
Scalability
Billing services can scale with practice growth without disrupting operations.
Regulatory Compliance
Staying compliant with changing mental health billing regulations reduces audit risks and penalties.
Mental Health Billing for Different Provider Types
Mental health billing services support a wide range of providers, including:
-
Psychiatrists
-
Psychologists
-
Licensed Clinical Social Workers (LCSWs)
-
Licensed Professional Counselors (LPCs)
-
Marriage and Family Therapists (MFTs)
-
Behavioral health clinics
-
Substance abuse treatment centers
-
Tele-mental health providers
Each provider type has unique billing requirements that specialized billing services can handle efficiently.
Learn more about mental health billing services and how they support behavioral health providers with accurate coding, compliance, and faster reimbursements.
Telehealth and Mental Health Billing
Tele-mental health services have become an essential part of behavioral healthcare. However, billing for telehealth requires:
-
Correct place-of-service (POS) codes
-
Telehealth modifiers (such as 95 or GT)
-
Payer-specific policies
-
State licensing considerations
Mental health billing services ensure telehealth claims are billed correctly and reimbursed at appropriate rates.
Compliance and Regulatory Considerations
Mental health billing must comply with:
-
HIPAA regulations
-
Mental Health Parity and Addiction Equity Act (MHPAEA)
-
CMS and payer-specific billing rules
-
State-specific mental health regulations
Professional billing services continuously monitor regulatory changes to maintain compliance and protect providers from audits and fines.
How Mental Health Billing Services Improve Patient Experience
Transparent billing processes improve patient trust and satisfaction. Accurate eligibility verification, clear statements, and responsive billing support reduce confusion and financial stress for patients seeking mental health care.
Choosing the Right Mental Health Billing Service Provider
When selecting a mental health billing partner, providers should consider:
-
Experience in behavioral health billing
-
Certified coding professionals
-
Knowledge of payer policies
-
Transparent pricing models
-
Strong denial management processes
-
Secure billing systems
A reliable billing partner acts as an extension of the provider’s practice.
Conclusion
Mental health billing services are essential for the financial success of behavioral health practices. With complex coding requirements, strict compliance standards, and evolving payer rules, outsourcing billing to experienced professionals ensures accuracy, efficiency, and consistent revenue.
By partnering with a specialized mental health billing service provider, mental health professionals can reduce administrative stress, improve cash flow, remain compliant, and focus on delivering high-quality patient care. As the mental health landscape continues to evolve, professional billing support becomes a strategic investment in long-term practice growth.