Fatty pancreas has become an increasingly recognised health condition in recent years. Similar to fatty liver disease, it involves fat deposits forming within pancreatic tissue, disrupting its normal functions. In 2025, medical professionals are focusing more closely on how to manage this condition through advanced diagnostics, therapeutic innovation, and sustainable lifestyle changes.
Understanding Fatty Pancreas and Its Implications
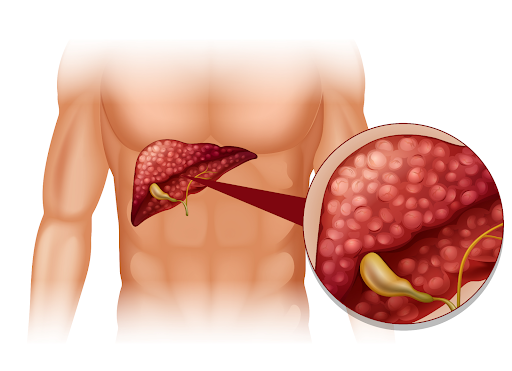
The pancreas plays a central role in digestion and blood sugar regulation. When excessive fat accumulates in the organ, a condition known as fatty pancreas, it can cause inflammation, interfere with enzyme production, and reduce insulin efficiency. Over time, these disruptions may increase the risk of diabetes, pancreatitis, or metabolic disorders.
The condition is often silent, showing minimal symptoms. Many individuals discover it incidentally during imaging tests for unrelated concerns. Studies now classify fatty pancreas as part of a larger metabolic syndrome, often linked to obesity, poor diet, and sedentary lifestyles.
The Rise of Diagnostic Precision
Medical imaging and technology have transformed how specialists identify pancreatic fat. Modern MRI scans and high-resolution ultrasounds can detect subtle changes in pancreatic tissue with remarkable accuracy. AI-supported image analysis tools introduced in 2025 are enhancing early detection and personalised treatment planning. Key diagnostic methods include:
- MRI and ultrasound: Identify fat infiltration in the pancreas.
- AI-based image evaluation: Improve precision in assessing disease extent.
- Biomarker analysis: Detect early signs of inflammation and organ stress.
Accurate diagnosis helps clinicians design early interventions and monitor recovery more effectively.
Lifestyle and Nutritional Interventions
Lifestyle correction remains the foundation of treatment. Small but consistent changes to diet and daily activity can reverse fat accumulation and restore pancreatic health. Effective strategies include:
- Balanced diet: Focus on whole grains, fruits, vegetables, and lean proteins.
- Healthy fats: Choose sources like olive oil, nuts, and omega-3-rich foods.
- Avoid processed foods: Limit trans fats, refined sugars, and packaged snacks.
- Weight management: Losing 5–10% of body weight can significantly improve outcomes.
- Regular exercise: Incorporate brisk walking, swimming, or yoga most days of the week.
These habits support overall metabolic health and complement any medical therapy recommended by healthcare professionals.
Medical Therapies and Clinical Trials
Ongoing research in 2025 is focusing on therapies that target the metabolic and inflammatory roots of fatty pancreas. Certain medications used in diabetes management, such as GLP-1 receptor agonists, are showing promise in reducing pancreatic fat. Other areas of research include:
- Antioxidants and anti-inflammatory agents: To reduce oxidative stress and tissue damage.
- Lipid-lowering drugs: To control fat deposition in organs.
- Hormonal therapies: To improve insulin sensitivity and enzyme function.
Clinical trials are underway to refine these treatments and determine which combinations deliver the most lasting benefits. Medical specialists continue to stress that drug therapy should always complement, not replace, lifestyle change.
The Role of Gut Health and the Microbiome
Growing evidence connects gut health to pancreatic function. An imbalance in gut bacteria can trigger inflammation and contribute to fat accumulation. Maintaining a healthy microbiome has therefore become an important part of modern management. Practical ways to support gut balance include:
- Consuming probiotic-rich foods such as yoghurt and fermented vegetables.
- Increasing fibre intake through fruits, vegetables, and whole grains.
- Reducing processed foods that can disrupt gut flora.
Although more research is required, a balanced gut environment appears to play a meaningful role in preventing pancreatic complications.
The Importance of Early Diagnosis and Monitoring
Because the condition develops gradually, early detection makes a substantial difference. People with obesity, diabetes, or a family history of metabolic diseases should undergo routine screenings. Recommended monitoring practices include:
- Regular imaging: MRI or ultrasound to assess changes in pancreatic tissue.
- Annual check-ups: Especially for those already diagnosed with fatty liver disease.
- Blood tests: To evaluate enzymes and inflammation markers.
Timely diagnosis helps prevent progression and ensures treatment plans remain effective and personalised.
Patient Awareness and Preventive Care
Awareness plays a crucial role in reducing disease burden. Educating patients about lifestyle choices, balanced nutrition, and early consultation can help prevent complications. Preventive healthcare programmes now encourage:
- Health education: Focused on diet, exercise, and risk awareness.
- Routine screening: For high-risk groups with metabolic issues.
- Holistic management: Combining nutrition, physiotherapy, and counselling.
Empowering individuals with knowledge and access to regular medical advice enables them to take control of their health before problems escalate.
The Road Ahead: Research and Hope
Medical research in 2025 continues to uncover new ways to manage and reverse fat accumulation in the pancreas. Developments in regenerative medicine, gene therapy, and personalised nutrition are bringing renewed optimism.
Collaborative global studies are analysing how genetics, lifestyle, and environment interact in metabolic diseases. The findings are expected to guide more targeted, effective, and less invasive treatments in the coming years.
Conclusion
Fatty pancreas is gaining recognition as a serious but manageable condition. With advancements in diagnostics, focused lifestyle changes, and ongoing medical innovation, managing it has become more achievable than ever.
Early intervention, balanced nutrition, and consistent follow-up remain the most reliable strategies for long-term pancreatic health. Preventive care and patient education continue to lead the way towards healthier outcomes in 2025 and beyond.