Introduction
Surgical power tools are indispensable in modern medical procedures, enabling precision and efficiency in surgeries. However, ensuring their safety and sterility is critical to preventing infections, improving patient outcomes, and maintaining compliance with healthcare regulations. Here we explore the best practices for maintaining the safety and sterility of surgical power tools.
Definition
Surgical power tools are specialized medical instruments powered by electricity, battery or compressed air, designed to assist surgeons in cutting, drilling, reaming, and shaping bone or soft tissue during surgical procedures. These tools enhance precision, reduce operative time, and improve patient outcomes in various medical fields, including orthopedics, neurology and cardiothoracic surgery.
Importance of Safety and Sterility
Surgical power tools, including drills, saws, and reamers, come into direct contact with patients’ tissues and bones. If not properly sterilized, they can serve as vectors for pathogens, leading to serious infections. Additionally, malfunctioning tools can compromise surgical precision, potentially causing harm to patients. Therefore, strict adherence to sterilization protocols and safety measures is necessary to uphold patient care standards.
Best Practices for Ensuring Safety in Surgical Power Tools
1. Proper Handling and Usage
- Train surgical staff on the correct operation of each tool.
- Use tools as per manufacturer guidelines to prevent mechanical failure.
- Regularly inspect tools before and after each procedure to ensure they are functioning correctly.
- Avoid excessive force or improper use, which can lead to damage or wear.
2. Routine Maintenance and Calibration
- Follow a strict maintenance schedule to keep tools in optimal working condition.
- Conduct routine calibrations to ensure precision and accuracy.
- Replace worn-out or damaged parts promptly to avoid unexpected malfunctions.
3. Battery and Power Source Management
- Use manufacturer-approved batteries and power sources.
- Monitor battery life and charge levels before procedures.
- Store batteries properly to prevent leakage or damage.
- Dispose of expired batteries following environmental safety guidelines.
4. Implementing Ergonomic Considerations
- Choose lightweight and ergonomically designed tools to reduce surgeon fatigue.
- Ensure comfortable grip and control to enhance precision.
- Minimize vibration levels to improve operational stability.
Best Practices for Sterilization of Surgical Power Tools
1. Pre-Cleaning Procedures
- Immediately after use, remove gross contaminants using an enzymatic detergent.
- Disassemble detachable parts as per manufacturer recommendations.
- Rinse thoroughly to eliminate residues before sterilization.
2. Appropriate Sterilization Methods
- Use sterilization techniques suitable for power tools, such as:
- Steam Sterilization (Autoclaving) – Effective for heat-resistant tools.
- Chemical Sterilization – Suitable for heat-sensitive components.
- Gas Plasma Sterilization – Ideal for complex instruments with small crevices.
- Dry Heat Sterilization – Effective for certain metal instruments.
3. Ensuring Compatibility with Sterilization Methods
- Check manufacturer guidelines to confirm the recommended sterilization process.
- Use protective barriers or sterilization pouches to maintain sterility.
- Avoid excessive exposure to heat or chemicals that may damage tool components.
4. Proper Storage and Handling Post-Sterilization
- Store sterilized tools in designated sterile areas.
- Use aseptic techniques when handling sterilized equipment.
- Monitor storage conditions, including temperature and humidity, to prevent contamination.
- Implement a clear labeling system to track sterilization dates and cycles.
Compliance with Regulatory Standards
- Adhere to guidelines set by regulatory bodies such as the FDA, CDC, and WHO.
- Ensure compliance with the hospital’s infection control policies.
- Conduct regular audits and training sessions to keep staff updated on best practices.
Challenges in Surgical Power Tools Market
High Cost of Surgical Power Tools:
Surgical power tools are expensive due to advanced technology and precision engineering. The high cost limits adoption, especially in small healthcare facilities and developing regions.
Stringent Regulatory Compliance:
Manufacturers must comply with strict regulations, including FDA and CE approvals. These requirements increase production costs and delay product launches, affecting market growth.
Risk of Infections and Safety Concerns:
Reusable surgical power tools require strict sterilization to prevent infections. Any lapse in hygiene protocols can lead to complications, making safety a primary concern.
Lack of Skilled Professionals:
Operating surgical power tools requires expertise. A shortage of trained surgeons and technicians, especially in emerging markets, hampers the effective use of these devices.
Intense Market Competition:
The market has numerous players, leading to price wars and reduced profit margins. This competition makes it difficult for smaller companies to sustain operations.
Increasing Demand for Minimally Invasive Surgery:
Traditional surgical power tools face competition from minimally invasive techniques. This shift in preference affects sales and requires manufacturers to adapt quickly.
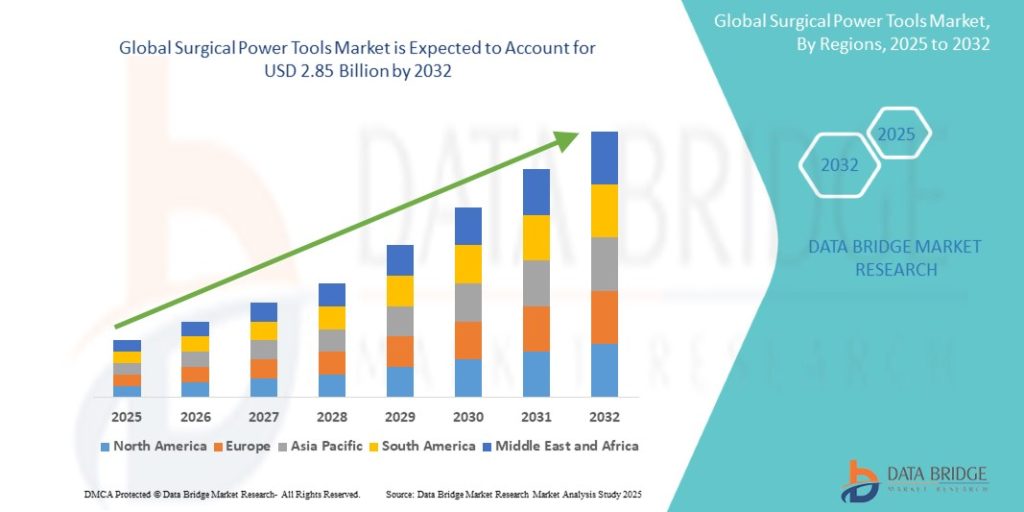
Growth Rate of Surgical Power Tools Market
According to Data Bridge Market Research, the surgical power tools market is expected to grow at a compound annual growth rate (CAGR) of 4.60% from 2025 to 2032, from its 2024 valuation of USD 1.99 billion to USD 2.85 billion.
Read More: https://www.databridgemarketresearch.com/reports/global-surgical-power-tools-market
Future Trends of the Surgical Power Tools Market
Increasing Demand for Minimally Invasive Surgery:
Minimally invasive procedures are gaining popularity. These surgeries require advanced power tools for smaller incisions, reduced recovery times, and minimal post-operative complications.
Integration of Robotics and AI:
Robotic-assisted surgeries are becoming mainstream. AI-powered tools enhance precision, allowing surgeons to perform complex procedures with improved accuracy and reduced fatigue.
Battery-Powered Surgical Tools:
Cordless, battery-operated surgical tools offer greater mobility. Enhanced battery life and quick charging features improve workflow, reducing dependency on wired power sources in operating rooms.
Advanced Materials and Durability:
Modern surgical power tools are designed with lightweight and durable materials. These tools ensure better ergonomics, reducing surgeon fatigue and increasing longevity.
Customization and Modular Designs:
Modular surgical tools allow customization based on procedure requirements. Surgeons can swap components, making tools versatile and cost-effective for various surgical applications.
Focus on Sterilization and Infection Control:
Hospitals prioritize infection control. Surgical power tools now feature improved sterilization techniques, ensuring compliance with stringent hygiene standards to prevent cross-contamination.
Smart Connectivity and Data Integration:
IoT-enabled surgical tools provide real-time data. These smart tools help monitor performance, offer predictive maintenance, and enhance overall surgical efficiency.
Conclusion
Ensuring the safety and sterility of surgical power tools is a crucial aspect of patient care. By following best practices in handling, maintenance, and sterilization, healthcare facilities can minimize infection risks and enhance surgical outcomes. Regular staff training and adherence to regulatory standards further support a culture of safety and excellence in surgical procedures.